Abstract
Review Article
Identifying patterns in COVID-19: Morbidity, recovery and the aftermath
Vinod Nikhra*
Published: 25 May, 2020 | Volume 4 - Issue 1 | Pages: 056-064
The infectivity and pathogenesis: SARS-CoV-2, the causative agent of Covid-19, involves Angiotensin-converting enzyme 2 (ACE2) receptors on type II alveolar type 2 (AT2) cells in lungs. Apart from, the upper and lower respiratory tracts, the disease affects the gastrointestinal system prominently, as evidenced by the significant GI symptoms, early in the course of the disease. In addition, the virus infects ACE2-bearing cells in other organs including the heart and blood vessels, brain, and kidneys.
Clinical features and morbidity: The clinical spectrum of COVID-19 varies from asymptomatic or pauci-symptomatic presentation to moderate to severe states characterized by respiratory failure necessitating mechanical ventilation and ICU support and those manifesting critical clinical condition with complications like sepsis, septic shock, and multiple organ dysfunction failure. The CT chest is an important tool for early identification of COVID-19 pneumonia as well as for prognostic purposes.
The recovery and residual damage: The recovery and other outcomes vary depending on age and other aspects including sex, comorbidities, and genetic factors. The outlook for older adults, who account for a disproportionate share of critical disease, is unfavorable, and most of those who survive are unlikely to return to their previous level of functioning. The disease affects their long-term health and quality of life as well as brings in propensity for truncated post-disease survival.
COVID-19 aftermath and follow up: The patients discharged from hospital following severe COVID-19, continue to suffer with lingering impact of the disease as well as that of the emergency treatments that saved their life. The post-infection reduced exercise tolerance and other subtle factors, like post viral fatigue syndrome, post-traumatic stress disorder, impaired concentration, delirium, and disturbed sleep-wake cycle often underly the functional impairment. In fact, there is need of step-down care and later a multidisciplinary support involving regular clinical assessment, respiratory review, physiotherapy, nutritional advice, and psychiatric support.
Conclusion: The life after COVID-19: After recovery from the disease, the virus SARS-CoV-2, may persist for uncertain period. In addition, the chance of reinfection cannot be ruled out. The vitamin D supplementation may be helpful. In general, the quality of life (QOL) in ICU survivors improves but remains lower than general population levels, but most of the patients adapt well to their level of self-sufficiency and QOL. Also, the debility due to co-morbidities may further compromise the activity of daily living and QOL issues. The Age and severity of illness appear to be the major predictors of post-discharge physical functioning.
Read Full Article HTML DOI: 10.29328/journal.ijcv.1001016 Cite this Article Read Full Article PDF
Keywords:
ACE2; Acute COVID-19 cardiovascular syndrome; Acute respiratory distress syndrome; COVID-19; Cytokine storm syndrome; SARS-CoV-2
References
- Zhao Y, Zhao Z, Wang Y. Single-cell RNA expression profiling of ACE2, the receptor of SARS-CoV-2. 2020.
- Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020; 7: 11. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32169119
- Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID‐19 and the possibility of faecal transmission. Alimentary Pharm & Thera. 2020; 51: 843-851. PubMed: https://onlinelibrary.wiley.com/doi/abs/10.1111/apt.15731?af=R
- Lamers MM, Beumer J, van der Vaart J, et al. SARS-CoV-2 productively infects human gut enterocytes. Science. 2020. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32358202
- Nikhra V. The Trans-zoonotic Virome interface: Measures to balance, control and treat epidemics. Ann Biomed Sci Eng. 2020; 4: 020-027.
- Guan WJ, Ni ZY, Hu Y, et al. For the China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020; 382: 1708-1720.
- McIntosh K, Hirsch MS, Bloom A. Coronavirus disease 2019 (COVID-19): Epidemiology, virology, clinical features, diagnosis, and prevention. Literature review current through: Mar 2020, last updated: 2020. https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19-epidemiology-virology-clinical-features-diagnosis-and-prevention
- Fu L, Wang B, Yuan T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis. J Infect. 2020, PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7151416/
- Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease in New York City. Intensive Care and Critical Care Medicine. 2020.
- Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020; 18: 844-847. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32073213
- Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 2020; 101623. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32179124
- Meng H, Xiong R, He R, Lin W, Hao B, et al. CT imaging and clinical course of asymptomatic cases with COVID-19 pneumonia at admission in Wuhan, China. J Infect. 2020. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32294504
- Hani C, Trieu NH, Saab I, S. Dangeard,a S. Bennani, et al. Thoracic imaging COVID-19 pneumonia: A review of typical CT findings and differential diagnosis. Diagnostic and Interventional Imaging. 2020; 101: 263-268. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7129663/
- Pan F, Ye T, Sun P, Gui S, Liang B. et al. Time Course of Lung Changes on Chest CT During Recovery From 2019 Novel Coronavirus (COVID-19). Radiology. 2020; 295: 715-721. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32053470
- Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 Patients. AJR Am J Roentgenol. 2020; 1-7. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32174129
- Murthy S, Gomersall CD, Fowler RA. Care for Critically Ill Patients with COVID-19. JAMA. 2020; 323: 1499-1500. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32159735
- Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020; PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32291094
- Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, et al. Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. NEJM Corres. 2020. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32343504
- Chen C, Zhou Y, Wang DW. SARS-CoV-2: a potential novel etiology of fulminant myocarditis. Herz. 2020; 45: 230-232. PubMed: https://pubmed.ncbi.nlm.nih.gov/32140732/
- Hendren NS, Drazner MH, Bozkurt B, Cooper LT, Jr. Description and Proposed Management of the Acute COVID-19 Cardiovascular Syndrome. Circulation. 2020.
- Yu Y, Shu H, Xia J, Shu H, Xia J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Resp Med. 2020; 8: P475-481. PubMed: https://pubmed.ncbi.nlm.nih.gov/32105632/
- Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, et al. Covid-19 in Critically Ill Patients in the Seattle Region - Case Series. NEJM. 2020. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32227758
- Gattinoni L, Chiumello D, Rossi S. COVID-19 pneumonia: ARDS or not?. Crit Care. 24; 154. 2020. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32299472
- Maiolo G, Collino F, Vasques F, Rapetti F, Tonetti T, et al. Reclassifying acute respiratory distress syndrome. Am J Respir Crit Care Med. 2018; 197: 1586–1595. https://www.ncbi.nlm.nih.gov/pubmed/29345967
- Henrya BM, Lippib G. Poor survival with extracorporeal membrane oxygenation in acute respiratory distress syndrome (ARDS) due to coronavirus disease 2019 (COVID-19): Pooled analysis of early reports. J Crit Care. 2020. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7118619/
- Porter DL, Maloney DG. Cytokine release syndrome (CRS). UpToDate. Retrieved from https://www.uptodate.com/contents/cytokine-release-syndrome-crs? 2020.
- Jose RJ, Manuel A. COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Resp Med Corres. 2020, PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32353251
- Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020; 18: 844-847. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32073213
- Tang N, Huan B, Xing C, Gong J, Li D, et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020; 18: 1094–1099. https://www.ncbi.nlm.nih.gov/pubmed/32220112
- Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 2020. https://www.who.int/publications-detail/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19)
- Porcheddu R, Serra C, Kelvin D, Kelvin N, Rubino S. Similarity in Case Fatality Rates (CFR) of COVID19/SARS-COV-2 in Italy and China. J Infect Dev Ctries. 2020; 14: 125–128. https://www.ncbi.nlm.nih.gov/pubmed/32146445
- Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32320003
- Zhou F, Yu T, Du R, Fan G, Liu Y, et al. Clinical course and risk factors for mortality of adult inpatients with COVID19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020; 395: 1054–1062. https://www.ncbi.nlm.nih.gov/pubmed/32171076
- Perez-Guzman PNP, Daunt A, Mukherjee S. Report 17: Clinical characteristics and predictors of outcomes of hospitalised patients with COVID-19 in a London NHS Trust: a retrospective cohort study. Imperial College COVID-19 response team. 2020.
- Vincent JL, Taccone FS. Understanding pathways to death in patients with COVID-19. Lancet Respir Med. 2020; 8: 430-432. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32272081
- Harrison DA, Parry GJ, Carpenter JR, Short A, Rowan K. A new risk prediction model for critical care: The Intensive Care National Audit & Research Centre (ICNARC) model. Crit Care Med. 2007; 35: 1091-1098. https://www.ncbi.nlm.nih.gov/pubmed/17334248
- Which breathing techniques help with COVID-19? Official Q & A. Medically reviewed by Drugs.com https://www.drugs.com/medical-answers/breathing-techniques-covid-19-3536315/
- Harman EM. Ed. Pinsky MR. What are the disadvantages to mechanical ventilation in the treatment of acute respiratory distress syndrome (ARDS)? Drugs & Diseases > Critical Care > Acute Respiratory Distress Syndrome (ARDS) Q&A. 2020. https://www.medscape.com/answers/165139-43338/what-are-the-disadvantages-to-mechanical-ventilation-in-the-treatment-of-acute-respiratory-distress-syndrome-ards.
- Mak IWC, Chu CM, Pan PC, Yiu MGC, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009; 31: 318–326. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19555791
- Guidance for stepdown of infection control precautions within hospitals and discharging COVID-19 patients from hospital to home settings. 2020. https://icmanaesthesiacovid-19.org/news/stepdown-of-infection-control-precautions-and-discharging-covid-19-patients-to-home-settings.
- Tabah A, Philippart F, Timsit JF, Willems V, Français A, et al. Quality of life in patients aged 80 or over after ICU discharge. Crit Care. 2010; 14: R2. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20064197
- Zhou F, Yu T, Du R, Fan G, Liu Y, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020; 395: 1054-1062, PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32171076
- Chen Y, Bai W, Liu B, et al. Re-evaluation of Nucleic Acid Retested Positive Cases in the Recovered COVID-19 Patients: Report from a Designated Transfer Hospital in Chongqing, China. 2020.
- Martineau AR, Jolliffe DA, Greenberg L, Greenberg L, Aloia JF, et al. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis. Health Technol Assess. 2019; 356: i6583. PubMed: https://pubmed.ncbi.nlm.nih.gov/28202713/
- Ilie PC, Stefanescu S, Smith L. The role of Vitamin D in the prevention of Coronavirus Disease 2019 infection and mortality. Research Squqre. 2020.
- Dowdy DW, Eid MP, Sedrakyan A, Mendez-Tellez PA, Pronovost PJ, et al. Quality of life in adult survivors of critical illness: a systematic review of the literature. Intensive Care Med. 2005’ 31: 611-620. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15803303
Figures:

Figure 1
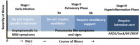
Figure 2

Figure 3

Figure 4
Similar Articles
-
Hypothesis about pathogenic action of Sars-COV-2Del Prete Salvatore*,Marasco Daniela,Sabetta Rosalaura. Hypothesis about pathogenic action of Sars-COV-2. . 2020 doi: 10.29328/journal.ijcv.1001009; 4: 021-022
-
The Psychology of the Common Cold and Influenza: Implications for COVID-19Andrew P Smith*. The Psychology of the Common Cold and Influenza: Implications for COVID-19. . 2020 doi: 10.29328/journal.ijcv.1001011; 4: 027-031
-
Yemen is free of COVID-19Hussein O Kadi*. Yemen is free of COVID-19. . 2020 doi: 10.29328/journal.ijcv.1001012; 4: 032-033
-
Exploring pathophysiology of COVID-19 infection: Faux espoir and dormant therapeutic optionsVinod Nikhra*. Exploring pathophysiology of COVID-19 infection: Faux espoir and dormant therapeutic options. . 2020 doi: 10.29328/journal.ijcv.1001013; 4: 034-040
-
COVID-19: Targeting the cytokine storm via cholinergic anti-inflammatory (Pyridostigmine)Ahmed H Osman*. COVID-19: Targeting the cytokine storm via cholinergic anti-inflammatory (Pyridostigmine). . 2020 doi: 10.29328/journal.ijcv.1001014; 4: 041-046
-
Identifying patterns in COVID-19: Morbidity, recovery and the aftermathVinod Nikhra*. Identifying patterns in COVID-19: Morbidity, recovery and the aftermath. . 2020 doi: 10.29328/journal.ijcv.1001016; 4: 056-064
-
Role of nanotechnology in diagnosing and treating COVID-19 during the PandemicAbdul Baset*,Abdul Waris,Muhammad Ali,Atta Ullah Khan,Asmat Ali. Role of nanotechnology in diagnosing and treating COVID-19 during the Pandemic. . 2020 doi: 10.29328/journal.ijcv.1001017; 4: 065-070
-
COVID-19: The possible medical strategiesMohamed SA Mohamed*. COVID-19: The possible medical strategies. . 2020 doi: 10.29328/journal.ijcv.1001018; 4: 071-075
-
Can house flies mechanically carry and/or transport sars-cov-2?Alfredo Montes*,Wilfrido Coronell,Rosa Baldiris. Can house flies mechanically carry and/or transport sars-cov-2?. . 2020 doi: 10.29328/journal.ijcv.1001019; 4: 076-078
-
Inhaled statins to combat COVID-19 – prophylactic and treatment approachArchana P Iyer*,Maryam A Al-Ghamdi. Inhaled statins to combat COVID-19 – prophylactic and treatment approach. . 2020 doi: 10.29328/journal.ijcv.1001020; 4: 079-080
Recently Viewed
-
Relationship between Vitamin D Deficiency and Lipopolysaccharides Porphyromonas gingivalis Bacteria in Stunting ChildrenErwin Gunawan*,Ria Puspitawati. Relationship between Vitamin D Deficiency and Lipopolysaccharides Porphyromonas gingivalis Bacteria in Stunting Children. Ann Biomed Sci Eng. 2024: doi: 10.29328/journal.abse.1001033; 8: 059-065
-
Addiction to self-strangulation: a case-reportAurely Ameller*,Yann Le Strat,Marion Cadranel,Celine Portalier, Caroline Dubertret. Addiction to self-strangulation: a case-report . J Addict Ther Res. 2017: doi: 10.29328/journal.jatr.1001003; 1: 016-021
-
Nanoencapsulated Extracts from Leaves of Bauhinia forficata Link: In vitro Antioxidant, Toxicogenetic, and Hypoglycemic Activity Effects in Streptozotocin-induced Diabetic MiceBárbara Verônica Cardoso de Souza, Alessandra Braga Ribeiro*, Rita de Cássia Meneses Oliveira, Julianne Viana Freire Portela, Ana Amélia de Carvalho Melo Cavalcante, Esmeralda Maria Lustosa Barros, Luís Felipe Lima Matos, Tarsia Giabardo Alves, Maria. Nanoencapsulated Extracts from Leaves of Bauhinia forficata Link: In vitro Antioxidant, Toxicogenetic, and Hypoglycemic Activity Effects in Streptozotocin-induced Diabetic Mice. Arch Pharm Pharma Sci. 2024: doi: 10.29328/journal.apps.1001063; 8: 100-115
-
Oral Suspension as Versatile Galenic Formulation in PediatryMauro Luisetto*, Almukthar N, Edbey K, Mashori GR, Fiazza C, Dona’ l, Cabianca L, Latyshev O. Oral Suspension as Versatile Galenic Formulation in Pediatry. Arch Pharm Pharma Sci. 2024: doi: 10.29328/journal.apps.1001062; 8: 091-099
-
Modulation of Microbiota and its Impact on DepressionKousik Maparu*. Modulation of Microbiota and its Impact on Depression. Arch Pharm Pharma Sci. 2024: doi: 10.29328/journal.apps.1001061; 8: 089-090
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."