Abstract
Review Article
Living with ‘Long COVID-19’: The long-term complications and sequelae
Vinod Nikhra*
Published: 16 February, 2021 | Volume 5 - Issue 1 | Pages: 011-021
Introduction - the perennial pandemic: It is being increasingly realised that the COVID-19 may have become the new reality associated with human existence world over and the mankind may have to live with it for years or even decades. Further, the grievous nature of the disease is evolving further with the genomic changes in the virus in form of mutations and evolution of variants, with enhanced infectivity and probably virulence. There are serious challenges posed by the SARS-CoV-2 virus and COVID-19 as the disease.
COVID-19 as acute and chronic disease: On exposure to the SARS-CoV-2 virus, not all patients develop a disease. Further, for those who develop the disease, there is a large variation in disease severity. The known factors including the constituent factors and several still unknown factors influence the disease manifestations, its course, and later the convalescent phase as well. In fact, substantial continuing morbidity after resolution of the infection indicates persisting multisystem effects of COVID-19.
The ‘long COVID-19’ or ‘long haulers’: The patients who continue to suffer with persisting symptoms have been described as long haulers and the clinical condition has been called post-COVID-19 or ‘long COVID-19’. The diagnosis should be entertained if various symptoms and signs linger well beyond the period of convalescence in COVID-19. With the chronicity, there occur inflammatory changes and damage in various organs, and the extent of organ damage determines the long-term effects.
Management of ‘long COVID’ syndrome: The ‘long COVID’ syndrome has multi-system involvement, variable presentation, and unpredictable course. Following clinical and investigational assessment, the patients should be managed as per clinical manifestations, extent of organ damage and associated complications. The findings from various studies indicate that preventing further organ damage in ‘long COVID’ is crucial.
The long COVID’s prognostic challenges: As apparent, the ‘long COVID’ afflictions are more common than realized earlier. The symptoms can escalate in patients with co-morbid conditions. The persistent symptoms among COVID-19 survivors pose new challenges to the healthcare providers and may be suitably managed with a combination of pharmacological and non-pharmacological treatments, and holistic healthcare.
Read Full Article HTML DOI: 10.29328/journal.ijcv.1001030 Cite this Article Read Full Article PDF
Keywords:
COVID-19; Long COVID; Long haulers; Post-COVID myocarditis; Pulmonary fibrosis; Brain fog; Chronic fatigue syndrome; Holistic care
References
- Max Planck Institute for the Science of Human History. COVID-19 is here to stay for the foreseeable future: Future of field-based sciences in the time of coronavirus. ScienceDaily. ScienceDaily, 14 September 2020. www.sciencedaily.com/releases/2020/09/200914112206.htm.
- Nikhra V. Exploring COVID-19: Relating the Spike Protein to Infectivity, Pathogenicity, and Immunogenicity. Research Gate. 2021.
- Oran DP, Topol EJ. The Proportion of SARS-CoV-2 Infections That Are Asymptomatic. Ann Internal Med. 2021.
- Pollitt KJG, Peccia J, Ko AI, Kaminski N, Cruz CSD, et al. COVID-19 vulnerability: the potential impact of genetic susceptibility and airborne transmission. Human Genomics. Hum Genomics. 2020; 14: 17. PubMed: https://pubmed.ncbi.nlm.nih.gov/32398162/
- Murray MF, Kenny EE, Ritchie MD, Rader DJ, Bale AE, et al. COVID-19 outcomes and the human genome. Gen Med. 2020; 22: 1175–1177. PubMed: https://pubmed.ncbi.nlm.nih.gov/32393819/
- Wu BB, Gu DZ, Yu JN, Yang J, Shen WQ. Association between ABO blood groups and COVID-19 infection, severity and demise: A systematic review and meta-analysis. Infect Genet Evol. 2020; 84: 104485. PubMed: https://pubmed.ncbi.nlm.nih.gov/32739464/
- Nguyen A, David JK, Maden SK. Human Leukocyte Antigen Susceptibility Map for Severe Acute Respiratory Syndrome Coronavirus 2. J Virol. 2020; 94: e00510-20.
- Project Leader Dr Helen Su, National Institute of Allergy and Infectious Diseases (NIAID)/National Institutes of Health (NIH), Bethesda, USA and Co-leader Dr Jean-Laurent Casanova, The Rockefeller University, Howard Hughes Medical Institute (HHMI), New York, USA and Necker Hospital for Sick Children & INSERM, Paris, France. https://www.COVIDhge.com
- Carfì A, Bernabei R, Landi F. Gemelli against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020; 324: 603-605. PubMed: https://pubmed.ncbi.nlm.nih.gov/32644129/
- Godlee F. Editors’s Choice - Living with COVID-19. BMJ. 2020; 370: m3392.
- del Rio C, Collins LF, Malani P. Long-term health consequences of COVID-19. JAMA. 2020. PubMed: https://pubmed.ncbi.nlm.nih.gov/33031513/
- Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of Long-COVID: analysis of COVID cases and their symptoms collected by the COVID Symptoms Study App. medRxiv and bioRxiv. 2020.
- Cellai M, O’Keefe JB. Characterization of prolonged COVID-19 symptoms and patient comorbidities in an outpatient telemedicine cohort. medRxiv and bioRxiv. 2020.
- Huang C, Huang L, Wang Y, Li X, Ren L, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021; 397: 220-232. PubMed: https://pubmed.ncbi.nlm.nih.gov/33428867/
- Weerahandi H, Hochman KA, Simon E, Blaum C, Chodosh J, et al. Post-discharge health status and symptoms in patients with severe COVID-19. Preprint. medRxiv. 2020; 2020; 08.11.20172742. PubMed: https://pubmed.ncbi.nlm.nih.gov/32817973/
- Davis HE, Assaf GS, McCorkell Ll. Characterizing Long COVID in an International Cohort: 7 Months of Symptoms and Their Impact. medRxiv preprint. 2020.
- Otte MS, Klussmann JP, Luers JC. Persisting olfactory dysfunction in patients after recovering from COVID-19. J Infect. 2020. 81: e58. PubMed: https://pubmed.ncbi.nlm.nih.gov/32592702/
- Paderno A, Mattavelli D, Rampinelli V, Grammatica A, Raffetti E, et al. Olfactory and Gustatory Outcomes in COVID-19: A Prospective Evaluation in Non-hospitalized Subjects. Otolaryngol Head Neck Surg. 2020; 163: 1144-1149. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7331108/
- Carvalho-Schneider C, Laurent E, Lemaignenet A, Beaufils E, Bourbao-Tournois C, et al., Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin Microbiol Infect. 2020; S1198-743X(20)30606-6. PubMed: https://pubmed.ncbi.nlm.nih.gov/33031948/
- Wise J. COVID-19: Symptoms are common after acute phase of disease, Italian study shows. BMJ. 2020; 370: m2804. PubMed: https://pubmed.ncbi.nlm.nih.gov/32651164/
- Ngai JC, Ko FW, Ng SS, Kin-Wang T, Tong M, et al. The long-term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status. Respirology. 2010; 15: 543-550. PubMed: https://pubmed.ncbi.nlm.nih.gov/20337995/
- Fraser E. Long term respiratory complications of COVID-19. BMJ. 2020; 370: m3001. PubMed: https://pubmed.ncbi.nlm.nih.gov/32747332/
- Huang Y, Tan C, Wu J, Chen M, Wang Z, et al. Impact of coronavirus disease 2019 on pulmonary function in early convalescence phase. Respir Res. 2020; 21: 163. PubMed: https://pubmed.ncbi.nlm.nih.gov/32600344/
- Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19) imaging reporting and data system (COVID-RADS) and common lexicon: a proposal based on the imaging data of 37 studies. Eur Radiol. 2020; 30: 4930-4942. PubMed: https://pubmed.ncbi.nlm.nih.gov/32346790/
- Zhao YM, Shang YM, Song WB, Qing-Quan L, Xie H, et al. Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery. eClinicalMedicine. 2020; 100463.
- Marshall M. The lasting misery of coronavirus long-haulers. Nature. 2020; 585: 339-341. PubMed: https://pubmed.ncbi.nlm.nih.gov/32929257/
- The prospective follow-up study of patients infected with the coronavirus, presented at the European Respiratory Society International Congress. 2020. https://www.ersnet.org/the-society/news/COVID-19-patients-suffer-long-term-lung-and-heart-damage-but-it-can-improve-with-time
- Leulseged TW, Hassen IS, Edo MG, et al. Duration of Supplemental Oxygen Requirement and Predictors in Severe COVID-19 Patients in Ethiopia: A Survival Analysis. medRxiv preprint. 2020.
- Zhang P, Li J, Liu H, Han N, Ju J, et al. Long-term bone and lung consequences associated with hospital-acquired severe acute respiratory syndrome: a 15-year follow-up from a prospective cohort study. Bone Res. 2020; 8: 34.
- Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020; 5: 1265-1273. PubMed: https://pubmed.ncbi.nlm.nih.gov/32730619/
- Sardari A, Tabarsi P, Borhany H, Mohiaddin R, Houshmand G. Myocarditis detected after COVID-19 recovery. Eur Heart J Cardiovasc Imaging. 2021; 22: 131-132. PubMed: https://pubmed.ncbi.nlm.nih.gov/32462177/
- Li B, Yang J, Zhao F, Zhi L, Wang X, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020; 109: 531-538. PubMed: https://pubmed.ncbi.nlm.nih.gov/32161990/
- Long B, Brady WJ, Koyfman A, Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020; 38: 1504-1507. PubMed: https://pubmed.ncbi.nlm.nih.gov/32317203/
- Eiros R, Barreiro-Perez M, Martin-Garcia A. Pericarditis and myocarditis long after SARS-CoV-2 infection: a cross-sectional descriptive study in health-care workers. medRxiv and bioRxiv preprint. 2020.
- Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, et al. CoroNerve Study Group. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. 2020; 7: 875-882. PubMed: https://pubmed.ncbi.nlm.nih.gov/32593341/
- Meppiel E, Peiffer-Smadja N, Maury A, Bekri I, Delorme C, et al. Neurologic manifestations associated with COVID-19: a multicentre registry. Clin Microbiol Infect. 2020. PubMed: https://pubmed.ncbi.nlm.nih.gov/33189873/
- Lyons D, Frampton M, Naqvi S, Donohoe D, Adams G, Glynn K. Fallout from the COVID-19 pandemic - should we prepare for a tsunami of post viral depression? Ir J Psychol Med. 2020; 37: 295-300. PubMed: https://pubmed.ncbi.nlm.nih.gov/32408926/
- Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, et al. Endothelial cell infection and endothelitis in COVID-19. Lancet. 2020; 95: 1417-1418. PubMed: https://pubmed.ncbi.nlm.nih.gov/32325026/
- Xiong TY, Redwood S, Prendergast B, Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020; 41: 1798-1800. PubMed: https://pubmed.ncbi.nlm.nih.gov/32186331/
- Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L, et al. Management of post-acute COVID-19 in primary care. BMJ. 2020; 370: m3026. PubMed: https://pubmed.ncbi.nlm.nih.gov/32784198/
- Salman D, Vishnubala D, Le Feuvre P, Beaney T, Korgaonkar J, et al. Returning to physical activity after COVID-19. BMJ. 2021; 372: m4721. PubMed: https://pubmed.ncbi.nlm.nih.gov/33419740/
- Tenforde MW, Kim SS, Lindsell CJ, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network-United States, March-June 2020. MMWR Morb Mortal Wkly Rep. 2020; 69: 993-998.
- Williams N. The Borg Rating of Perceived Exertion (RPE) scale. Occup Med. 2017; 67: 404-405.
- Nabavi N. COVID-19: Consider overall impact of long COVID symptoms when deciding whether to refer, says NICE. BMJ. 2020; 371: m4915.
- National Institute for Health and Care Excellence. COVID-19 rapid guideline: managing the long-term effects of COVID-19. 2020. www.nice.org.uk/guidance/ng188.
- Ting R, Edmonds P, Higginson IJ, Sleeman KE. Palliative care for patients with severe COVID-19. BMJ. 2020; 370: m2710. PubMed: https://pubmed.ncbi.nlm.nih.gov/32665316/
- Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L, et al. Management of post-acute COVID-19 in primary care. BMJ. 2020; 370: m3026. PubMed: https://pubmed.ncbi.nlm.nih.gov/32784198/
- Halpin, SJ, McIvor, C, Whyatt, G, Adams A, Harvey O, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J Med Virol. 2021; 93: 1013-1022. PubMed: https://pubmed.ncbi.nlm.nih.gov/32729939/
- Late Sequelae of COVID-19. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/late-sequelae.html
Figures:
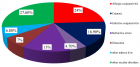
Figure 1

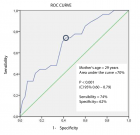
Figure 2
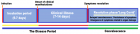
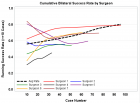
Figure 3

Figure 4
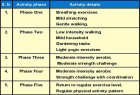
Figure 5
Similar Articles
-
Pseudoephedrine protects mice from infection of H1N1 virusZhongping Wu*,Li Deng,Chengzhi Chu,Xiaoyin Chen*. Pseudoephedrine protects mice from infection of H1N1 virus. . 2020 doi: 10.29328/journal.ijcv.1001008; 4: 014-020
-
The Psychology of the Common Cold and Influenza: Implications for COVID-19Andrew P Smith*. The Psychology of the Common Cold and Influenza: Implications for COVID-19. . 2020 doi: 10.29328/journal.ijcv.1001011; 4: 027-031
-
Yemen is free of COVID-19Hussein O Kadi*. Yemen is free of COVID-19. . 2020 doi: 10.29328/journal.ijcv.1001012; 4: 032-033
-
Exploring pathophysiology of COVID-19 infection: Faux espoir and dormant therapeutic optionsVinod Nikhra*. Exploring pathophysiology of COVID-19 infection: Faux espoir and dormant therapeutic options. . 2020 doi: 10.29328/journal.ijcv.1001013; 4: 034-040
-
COVID-19: Targeting the cytokine storm via cholinergic anti-inflammatory (Pyridostigmine)Ahmed H Osman*. COVID-19: Targeting the cytokine storm via cholinergic anti-inflammatory (Pyridostigmine). . 2020 doi: 10.29328/journal.ijcv.1001014; 4: 041-046
-
Identifying patterns in COVID-19: Morbidity, recovery and the aftermathVinod Nikhra*. Identifying patterns in COVID-19: Morbidity, recovery and the aftermath. . 2020 doi: 10.29328/journal.ijcv.1001016; 4: 056-064
-
Role of nanotechnology in diagnosing and treating COVID-19 during the PandemicAbdul Baset*,Abdul Waris,Muhammad Ali,Atta Ullah Khan,Asmat Ali. Role of nanotechnology in diagnosing and treating COVID-19 during the Pandemic. . 2020 doi: 10.29328/journal.ijcv.1001017; 4: 065-070
-
COVID-19: The possible medical strategiesMohamed SA Mohamed*. COVID-19: The possible medical strategies. . 2020 doi: 10.29328/journal.ijcv.1001018; 4: 071-075
-
Inhaled statins to combat COVID-19 – prophylactic and treatment approachArchana P Iyer*,Maryam A Al-Ghamdi. Inhaled statins to combat COVID-19 – prophylactic and treatment approach. . 2020 doi: 10.29328/journal.ijcv.1001020; 4: 079-080
-
A Comprehensive review on genomic diversity and epidemiology of COVID-19Zeshan Haider Raza*,Muhammad Ahmed Ihsan,Sahrish Khan,Haroon Zafar,Tayyaba Rehman. A Comprehensive review on genomic diversity and epidemiology of COVID-19. . 2020 doi: 10.29328/journal.ijcv.1001021; 4: 081-095
Recently Viewed
-
Relationship between Vitamin D Deficiency and Lipopolysaccharides Porphyromonas gingivalis Bacteria in Stunting ChildrenErwin Gunawan*,Ria Puspitawati. Relationship between Vitamin D Deficiency and Lipopolysaccharides Porphyromonas gingivalis Bacteria in Stunting Children. Ann Biomed Sci Eng. 2024: doi: 10.29328/journal.abse.1001033; 8: 059-065
-
Addiction to self-strangulation: a case-reportAurely Ameller*,Yann Le Strat,Marion Cadranel,Celine Portalier, Caroline Dubertret. Addiction to self-strangulation: a case-report . J Addict Ther Res. 2017: doi: 10.29328/journal.jatr.1001003; 1: 016-021
-
Nanoencapsulated Extracts from Leaves of Bauhinia forficata Link: In vitro Antioxidant, Toxicogenetic, and Hypoglycemic Activity Effects in Streptozotocin-induced Diabetic MiceBárbara Verônica Cardoso de Souza, Alessandra Braga Ribeiro*, Rita de Cássia Meneses Oliveira, Julianne Viana Freire Portela, Ana Amélia de Carvalho Melo Cavalcante, Esmeralda Maria Lustosa Barros, Luís Felipe Lima Matos, Tarsia Giabardo Alves, Maria. Nanoencapsulated Extracts from Leaves of Bauhinia forficata Link: In vitro Antioxidant, Toxicogenetic, and Hypoglycemic Activity Effects in Streptozotocin-induced Diabetic Mice. Arch Pharm Pharma Sci. 2024: doi: 10.29328/journal.apps.1001063; 8: 100-115
-
Oral Suspension as Versatile Galenic Formulation in PediatryMauro Luisetto*, Almukthar N, Edbey K, Mashori GR, Fiazza C, Dona’ l, Cabianca L, Latyshev O. Oral Suspension as Versatile Galenic Formulation in Pediatry. Arch Pharm Pharma Sci. 2024: doi: 10.29328/journal.apps.1001062; 8: 091-099
-
Modulation of Microbiota and its Impact on DepressionKousik Maparu*. Modulation of Microbiota and its Impact on Depression. Arch Pharm Pharma Sci. 2024: doi: 10.29328/journal.apps.1001061; 8: 089-090
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."