Abstract
Brief Communication
SARS-CoV-2 infection-associated detrimental effects on the various human organs
Haleema Nadeem, Mahnoor Ayesha, Umar Saeed*, Zahra Zahid Piracha, Rafia Tahir, Noor-Ul-Ain, Farrah Mehtab, Rida Fatima and Rizwan Uppal
Published: 26 October, 2021 | Volume 5 - Issue 2 | Pages: 072-081
The SARS-Cov-2 virus was firstly identified in Wuhan, China and caused catastrophic destruction all over the world. COVID-19 virus primarily effects lungs of its hosts and impairs it in number of ways. It can also damage multiple organs like Heart, kidney, endocrine glands, skin, brain and several others. Kidneys are also damaged to a great extent. In Heart it can cause acute coronary syndrome, Heart failure, Myocardial infarction. SARS-CoV-2 effect brain especially psychologically. It also causes serious lymphocyte apoptosis. It also neutralizes human spleen and lymph nodes. SARS-CoC-2 can be harmful for those having already liver diseases. Similarly, SARS-CoV-2 has a direct impact on endocrine glands. It is responsible for the various injurious changes in hormones, causes various diseases like acute pancreatitis, decrease in GH, hypoparathyroidism etc. and lead to cause tissues damage in glands. It also some minor effects on nose, and respiratory pathways. It also has some minor effects on eyes and ears whereas it causes several devastations in GIT.
Read Full Article HTML DOI: 10.29328/journal.ijcv.1001038 Cite this Article Read Full Article PDF
Keywords:
SARS-CoV-2; COVID-19; Heart; Brian; Lungs; Kidneys; Myocarditis; Conjuncti-vitis; Acute pancreatitis; COVID-19 acute respiratory syndrome; Lymph follicle exhaustion; Splenic knob; Histocyte hyperplasia; ACE
References
- Li Q, Guan X, Wu P, Wang X, Zhou L, et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020; 382: 1199-1207. PubMed: https://pubmed.ncbi.nlm.nih.gov/31995857/
- Bogoch A, Watts A, Thomas-Bachli C, Huber MUG, Kraemer K. Pneumonia of unknown etiology in wuhan, China: potential for international spread via commercial air travel. J Trav Med. 2020; 27: taaa008. PubMed: https://pubmed.ncbi.nlm.nih.gov/31943059/
- Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in wuhan China: the mystery and the miracle. J Med Virol. 2020; 92: 401-402. PubMed: https://pubmed.ncbi.nlm.nih.gov/31950516/
- How does coronavirus kill? Clinicians trace a fero. 2020..
- Jain U. Effect of COVID-19 on the Organs. Cureus. 2020; 12: e9540. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7470660/
- Mehta JL, Calcaterra G, Bassareo PP. COVID‐19, thromboembolic risk, and Virchow's triad: Lesson from the past. Clin Cardiol. 2020; 43: 1362-1367. PubMed: https://pubmed.ncbi.nlm.nih.gov/33176009/
- Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020; 17: 259-260.PubMed: https://pubmed.ncbi.nlm.nih.gov/32139904/
- Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020; 5: 819-824.PubMed: https://pubmed.ncbi.nlm.nih.gov/32219357/
- Ni W, Yang X, Yang D, Bao J, Li R, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care. 2020; 24: 1-10. PubMed: https://pubmed.ncbi.nlm.nih.gov/32660650/
- Wadman M, Couzin-Frankel J, Kaiser J, Matacic C. Rampage through the body, from brain to toes. 2020. PubMed: https://www.sciencemag.org/news/2020/04/how-does-coronavirus-kill-clinicians-trace-ferocious-rampage-through-body-brain-toes
- Guan WJ, Ni ZY, Hu YU, Liang WH, Ou CQ, et al. Clinical characteristics of coronavirus disease 2019 in China. New Eng J Med. 2020; 382: 1708–1720.
- Batiha O, Al‐Deeb T, Al‐zoubi EA, Alsharu E. Impact of COVID‐19 and other viruses on reproductive health. Andrologia. 2020; 52: e13791. PubMed: https://pubmed.ncbi.nlm.nih.gov/32790205/
- Fan C, Li K, Ding Y, Lu WL, Wang J. ACE2 expression in kidney and testis may cause kidney and testis damage after 2019-nCoV infection. MedRxiv. 2020.
- Wang Z, Xu X. scRNA-seq profiling of human testes reveals the presence of the ACE2 receptor, a target for SARS-CoV-2 infection in spermatogonia, leydig and sertoli Cells. Cells. 2020; 9: 920. PubMed: https://pubmed.ncbi.nlm.nih.gov/32283711/
- Darlenski R, Tsankov N. COVID-19 pandemic and the skin: what should dermatologists know? Clin Dermatol. 2020; 38: 785-787. PubMed: https://pubmed.ncbi.nlm.nih.gov/33341217/
- Foo CC, Goon ATJ, Leow YH, et al. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome--a descriptive study in Singapore. Contact Dermatitis. 2006; 55: 291–294. PubMed: https://pubmed.ncbi.nlm.nih.gov/17026695/
- Xia J, Tong J, Liu M, Shen Y, Guo D, et al. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020; 92: 589-594. PubMed: https://pubmed.ncbi.nlm.nih.gov/32100876/
- Zhou L, Xu Z, Castiglione G, et al. ACE2 and TMPRSS2 are expressed on the human ocular surface, suggesting susceptibility to SARS-CoV-2 infection. BioRxiv. 2020; 92: 589-594.PubMed: https://pubmed.ncbi.nlm.nih.gov/32100876/
- Wu P, Duan F, Luo C, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei province, China. JAMA Ophthalmol. 2020; 138: 575–578. PubMed: https://pubmed.ncbi.nlm.nih.gov/32232433/
- Seah I, Agrawal R. Can the coronavirus disease 2019 (COVID-19) affect the eyes? A review of coronaviruses and ocular implications in humans and animals. Ocul Immunol Inflamm. 2020; 28: 391-395. PubMed: https://pubmed.ncbi.nlm.nih.gov/32175797/
- Hung ECW, Chim SSC, Chan PKS, et al. Detection of SARS coronavirus RNA in the cerebrospinal fluid of a patient with severe acute respiratory syndrome. Clin Chem. 2003; 49: 2107–2108. PubMed: https://pubmed.ncbi.nlm.nih.gov/14633896/
- Lau K, Yu W, Chu C, Lau S, Sheng B. Possible central nervous system infection by SARS coronavirus. Emerg Infect Dis. 2004; 10: 342–344. PubMed: https://pubmed.ncbi.nlm.nih.gov/15030709/
- Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. 2020; 94: 55–58. PubMed: https://pubmed.ncbi.nlm.nih.gov/32251791/
- Wang J, Jiang M, Chen X, Montaner LJ. Cytokine storm and leukocyte changes in mild versus severe SARS-CoV-2 infection: review of 3,939 COVID-19 patients in China and emerging pathogenesis and therapy concepts. J Leukoc Biol. 2020; 108: 17–41. PubMed: https://pubmed.ncbi.nlm.nih.gov/32534467/
- Bullen CK, Hogberg HT, Bahadirli-Talbott A, Bishai WR, Hartung T, et al. Infectability of human BrainSphere neurons suggests neurotropism of SARS-CoV-2. ALTEX 37. 2020; 665–671. PubMed: https://pubmed.ncbi.nlm.nih.gov/32591839/
- Erickson MA, Banks WA. Neuroimmune axes of the blood–brain barriers and blood–brain interfaces: bases for physiological regulation, disease states and pharmacological interventions. Pharmacol Rev. 2018; 70: 278–314. PubMed: https://pubmed.ncbi.nlm.nih.gov/29496890/
- Buzhdygan TP, DeOre BJ, Baldwin-Leclair A, Bullock TA, McGary HM, et al. The SARS-CoV-2 spike protein alters barrier function in 2D static and 3D microfluidic in-vitro models of the human blood–brain barrier. Neurobiol Dis. 2020; 146: 105131. PubMed: https://pubmed.ncbi.nlm.nih.gov/33053430/
- Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, et al. Angiotensin-converting enzyme 2: a functional receptor for SARS coronavirus. Nature. 2003; 426: 450–454. PubMed: https://pubmed.ncbi.nlm.nih.gov/14647384/
- Hamming I, Timens W, Bulthuis MLC, Lely AT, Navis GJ, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004; 203: 631–637. PubMed: https://pubmed.ncbi.nlm.nih.gov/15141377/
- Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. 2008; 82: 7264–7275. PubMed: https://pubmed.ncbi.nlm.nih.gov/18495771/
- Ding Y, Wang H, Shen H, Li Z, Geng J, et al. The clinical pathology of severe acute respiratory syndrome (SARS): A report from China. J Pathol. 2003; 200: 282–289. PubMed: https://pubmed.ncbi.nlm.nih.gov/12845623/
- Chen R, Wang K, Yu J, Howard D, French L, et al. The spatial and cell-type distribution of SARS-CoV-2 receptor ACE2 in the human and mouse brains. Front Neurol. 2021; 11: 573095. PubMed: https://pubmed.ncbi.nlm.nih.gov/33551947/
- Gu J, Gong E, Zhang B, Zheng J, Gao Z, et al. Multiple organ infection and the pathogenesis of SARS. J Exp Med. 2005; 202: 415–424. PubMed: https://pubmed.ncbi.nlm.nih.gov/16043521/
- Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, et al. Neurologic Features in Severe SARS-CoV-2 Infection. N Engl J Med. 2020; 382: 2268–2270. PubMed: https://pubmed.ncbi.nlm.nih.gov/32294339/
- Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020; 383: 510-512.
- Feng Z, Diao B, Wang R, Wang G, Wang C, et al. The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) directly decimates human spleens and lymph nodes. MedRxiv. 2020.
- Peiris JS, Chu CM, Cheng VCC, Chan KS, Hung IFN, et al. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: A prospective study. Lancet. 2003; 361: 1767–1772. PubMed: https://pubmed.ncbi.nlm.nih.gov/12781535/
- Xu L, Liu J, Lu M, Yang D, Zheng X. Liver injury during highly pathogenic human coronavirus infections. Liver Int. 2020; 40: 998-1004.PubMed: https://pubmed.ncbi.nlm.nih.gov/32170806/
- Zhang C, Shi L, Wang FS. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020; 5: 428-430. PubMed: https://pubmed.ncbi.nlm.nih.gov/32145190/
- Yao XH, Li TY, He ZC, Ping YF, Liu HW, et al. A pathological report of three COVID-19 cases by minimal invasive autopsies. Chin J Pathol. 2020; 49: 411–417. PubMed: https://pubmed.ncbi.nlm.nih.gov/32172546/
- Wang F, Wang H, Fan J, Zhang Y, Wang HQ. Zhao Pancreatic injury patterns in patients with COVID-19 pneumonia Gastroenterology. 2020; 5: 434-435. PubMed: https://pubmed.ncbi.nlm.nih.gov/32247022/
- Inamdar S, Benias PC, Liu Y, Sejpal DV, Satapathy SK, et al. Prevalence, risk factors, and outcomes of hospitalized patients with COVID-19 presenting as acute pancreatitis. Gastroenterology. 2020; 159: 2226–2228.e2PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7448741/
- Al Mazrouei SS, Saeed GA, Al Helali AA. COVID-19-associated acute pancreatitis: a rare cause of acute abdomen. Radiol Case Rep. 2020; 15: 1601-1603. PubMed: https://pubmed.ncbi.nlm.nih.gov/32685078/
- Hadi A, Werge M, Kristiansen KT, Pedersen UG, Karstensen JG, et al. Coronavirus disease-19 (COVID-19) associated with severe acute pancreatitis: case report on three family members. Pancreatology. 2020; 20: 665-667. PubMed: https://pubmed.ncbi.nlm.nih.gov/32387082/
- de-Madaria E, Capurso G. COVID-19 and acute pancreatitis: examining the causality. Nature Reviews Gastroenterol Hepatol. 2021; 18: 3-4. PubMed: https://pubmed.ncbi.nlm.nih.gov/33203968/
- Liu F, Long X, Zou W, Fang M, Wu W, et al. Highly ACE2 expression in pancreas may cause pancreas damage after SARS-CoV-2 infection. 2020.
- Deisl C, Simonin A, Anderegg M, Albano G, Kovacs G, et al. Sodium/hydrogen exchanger NHA2 is critical for insulin secretion in β-cells. Proc Natl Acad Sci U S A. 2013; 110: 10004–10009. PubMed: https://pubmed.ncbi.nlm.nih.gov/23720317/
- Zhou L, Zhang M, Wang J, Gao J. Sars-Cov-2: underestimated damage to nervous system. Travel Med Infect Dis. 2020; 36: 101642. PubMed: https://pubmed.ncbi.nlm.nih.gov/32220634/
- Li T, Wang L, Wang H, Gao Y, Hu X, et al. Characteristics of laboratory indexes in COVID-19 patients with non-severe symptoms in Hefei City, China: diagnostic value in organ injuries. Eur J Clin Microbiol Infect Dis. 2020; 39: 2447-2455. PubMed: https://pubmed.ncbi.nlm.nih.gov/32613308/
- Christ Crain M, Hoorn EJ, Sherlock M, Thompson CJ, Wass JAH. Endocrinology in the time of COVID-19: management of Hyponatraemia and diabetes Insipidus. Eur J Endocrinol. 2020; 183: G9–G15. PubMed: https://pubmed.ncbi.nlm.nih.gov/32380474/
- Chen M, Zhou W, Xu W. Thyroid function analysis in 50 patients with COVID-19: a retrospective study. Thyroid. 2021; 31: 8-11.PubMed: https://pubmed.ncbi.nlm.nih.gov/32600165/
- Brancatella A, Ricci D, Viola N, Sgrò D, Santini F, et al. Subacute thyroiditis after sars-COV-2 infection. J Clin Endocrinol Metab. 2020; 105: dgaa276.PubMed: https://pubmed.ncbi.nlm.nih.gov/32436948/
- Gao W, Guo W, Guo Y, Shi M, Dong G, et al. Thyroid hormone concentrations in severely or critically ill patients with COVID-19. J Endocrinol Invest. 2021; 44: 1031-1040. PubMed: https://pubmed.ncbi.nlm.nih.gov/33140379/
- Lui DTW, Lee CH, Chow WS, Lee ACH, Tam AR, et al. Thyroid dysfunction in relation to immune profile, disease status and outcome in 191 patients with COVID-19. J Clin Endocrinol Metab. 2020. PubMed: https://pubmed.ncbi.nlm.nih.gov/33141191/
- Freire Santana M, Borba MGS, Baía-da-Silva DC, et al. Case report: adrenal pathology findings in severe COVID-19: an autopsy study. Am J Trop Med Hyg. 2020; 103: 1604–1607. PubMed: https://pubmed.ncbi.nlm.nih.gov/32876012/
- Liu J, Han P, Wu J, Gong J, Tian D. Prevalence and predictive value of hypocalcemia in severe COVID-19 patients. J Infect Public Health. 2020; 13: 1224–1228. PubMed: https://pubmed.ncbi.nlm.nih.gov/32622796/
- Elkattawy S, Alyacoub R, Ayad S, Pandya M, Eckman A. A novel case of hypoparathyroidism secondary to SARS-CoV-2 infection. Cureus. 2020; 12: e10097. PubMed: https://pubmed.ncbi.nlm.nih.gov/33005518/
- Bobaker A, Alzwi A. The effect of COVID-19 on parathyroid glands. J Infect Public Health. 2021; 14: 724-725. PubMed: https://pubmed.ncbi.nlm.nih.gov/34020212/
- Frankel M, Feldman I, Levine M, Frank Y, Bogot NR, et al. Bilateral adrenal hemorrhage in Coronavirus disease 2019 patient: a case report. J Clin Endocrinol Metab. 2020; 105: dgaa487.PubMed: https://pubmed.ncbi.nlm.nih.gov/32738040/
- Álvarez-Troncoso J, Zapatero Larrauri M, Montero Vega MD, et al. Case report: COVID-19 with bilateral adrenal hemorrhage. Am J Trop Med Hyg. 2020; 103: 1156-1157.PubMed: https://pubmed.ncbi.nlm.nih.gov/32682452/
- Ma L, Xie W, Li D, Shi L, Mao Y, et al. Effect of SARS-CoV-2 infection upon male gonadal function: a single center-based study. 2020. PubMed: https://medrxiv.org/lookup
- Muller I, Cannavaro D, Dazzi D, Covelli D, Mantovani G, et al. SARS-CoV-2-related atypical thyroiditis. Lancet Diabetes Endocrinol. 2020; 8: 739–741. PubMed: https://pubmed.ncbi.nlm.nih.gov/32738929/
- Channappanavar R, Fett C, Mack M, Ten Eyck PP, Meyerholz DK, et al. Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J Immunol. 2017; 198: 4046–4053. PubMed: https://pubmed.ncbi.nlm.nih.gov/28373583/
- Piticchio T, Le Moli R, Tumino D, Frasca F. Relationship between beta coronaviruses and the endocrine system: a new key to understand the COVID-19 pandemic—A comprehensive review. J Endocrinological Invest. 2021; 44: 1553-1570.. PubMed: https://pubmed.ncbi.nlm.nih.gov/33583003/
- Zhou F, Yu T, Du R, Fan G, Liu Y, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020; 395: 1054-1062. PubMed: https://pubmed.ncbi.nlm.nih.gov/32171076/
- Xu Z, Shi L, Wang Y, Zhang J, Huang L, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respirat Med. 2020; 8: 420-422. PubMed: https://pubmed.ncbi.nlm.nih.gov/32085846/
- Mo X, Jian W, Su Z, Chen M, Peng H, et al. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. Eur Respirat J. 2020; 55:PubMed: https://pubmed.ncbi.nlm.nih.gov/32381497/
- PubMed: https://www.lung.org/lung-health-diseases/lung-disease-lookup/ards
- Wu C, Chen X, Cai Y, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Internal Med. 2020; 180: 934-943. PubMed: https://pubmed.ncbi.nlm.nih.gov/32167524/
- PubMed: https://my.clevelandclinic.org/health/diseases/10959-pulmonary-fibrosis
- Liu X, Zhou H, Zhou Y, Wu X, Zhao Y, et al. Risk factors associated with disease severity and length of hospital stay in COVID-19 patients. J Infect. 2020; 81: e95-e97. PubMed: https://pubmed.ncbi.nlm.nih.gov/32305490/
- Rai DK, Sharma P, Kumar R. Post covid 19 pulmonary fibrosis-Is it real threat? Indian J Tuberculo. 2021; 68: 330-333.PubMed: https://pubmed.ncbi.nlm.nih.gov/34099197/
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, et al. Clinical characteristics of coronavirus disease 2019 in China. New Eng J Med. 2020; 382: 1708-1720.
- PubMed: https://www.kidney.org/atoz/content/AcuteKidneyInjury
- Xiao G, Hu H, Wu F, Sha T, Zeng Z, et al. Acute kidney injury in patients hospitalized with COVID-19 in Wuhan, China: a single-center retrospective observational study. J Southern Med Univers. 2021; 41: 157-163. PubMed: https://pubmed.ncbi.nlm.nih.gov/33624587/
- Benedetti C, Waldman M, Zaza G, Riella LV, Cravedi P. COVID-19 and the kidneys: an update. Front Med. 2020; 7: 423. PubMed: https://pubmed.ncbi.nlm.nih.gov/32793615/
- Pei G, Zhang Z, Peng J, Liu L, Zhang C, et al. Renal involvement and early prognosis in patients with COVID-19 pneumonia. J Am Soci Nephrol. 2020; 31: 1157-1165. PubMed: https://pubmed.ncbi.nlm.nih.gov/32345702/
- Noble R, Tan MY, McCulloch T, Shantier M, Byrne C, et al. Collapsing glomerulopathy affecting native and transplant kidneys in individuals with COVID-19. Nephron. 2020; 144: 589-594. PubMed: https://pubmed.ncbi.nlm.nih.gov/32894838/
- Li Z, Wu M, Yao J, Guo J, Liao X, et al. Caution on kidney dysfunctions of COVID-19 patients. 2020.
- Ostfeld E, Rubinstein E, Gazit E, Smetana Z. Effect of systemic antibiotics on the microbial flora of the external ear canal in hospitalized children. Pediatrics. 1977; 60: 364-366.
- Nguyen DK, Jueng J, Maul TM, Wei JL. Middle ear effusion prevalence at time of tympanostomy before and during COVID-19 pandemic. Int J Pediat Otorhinolaryngol. 2021; 147: 110785. PubMed: https://pubmed.ncbi.nlm.nih.gov/34116322/
- Umashankar A, Prabhu P. Effect of Covid-19 on Individuals with Hearing Impairment in India. J Clin Diagnos Res. 2020; 14.
- Ye G, Li Y, Lu M, Chen S, Luo Y, et al. Standardized Sampling by the Same Nurse Could Improve the Positive Rate and Consistency of the Throat Swabs to Detect COVID-19. 2020.
- Lai T, Xiang F, Zeng J, Huang Y, Jia L, et al. Reliability of induced sputum test is greater than that of throat swab test for detecting SARS-CoV-2 in patients with COVID-19: A multi-center cross-sectional study. Virulence. 2020; 11: 1394-1401. PubMed: https://pubmed.ncbi.nlm.nih.gov/33073676/
- Di Stadio A, Ralli M, Ricci G. Gender differences in COVID-19 infection. The estrogen effect on upper and lower airways. Can it help to figure out a treatment. Eur Rev Med Pharmacol Sci. 2020; 24: 5195-5196. PubMed: https://pubmed.ncbi.nlm.nih.gov/32495849/
- Gallo O. Risk for COVID-19 infection in patients with tobacco smoke-associated cancers of the upper and lower airway. Eur Arch Otorhinolaryngol. 2021; 278: 2695-2702. PubMed: https://pubmed.ncbi.nlm.nih.gov/33216184/
- Travis CR. As plain as the nose on your face: the case for a nasal (mucosal) route of vaccine administration for Covid-19 disease prevention. Front Immunol. 2020; 11: PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7561361/
- Han C, Duan C, Zhang S, Spiegel B, Shi H, et al. Digestive symptoms in COVID-19 patients with mild disease severity: clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol. 2020; 115: 916-923.PubMed: https://pubmed.ncbi.nlm.nih.gov/32301761/
- Parasa S, Desai M, Chandrasekar VT, Patel HK, Kennedy KF, et al. Prevalence of gastrointestinal symptoms and fecal viral shedding in patients with coronavirus disease 2019: a systematic review and meta-analysis. JAMA Network Open. 2020; 3: e2011335-e2011335. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7290409/
- Almeida JFMD, Chehter EZ. COVID-19 and the gastrointestinal tract: what do we already know? Einstein (Sao Paulo). 2020; 18:PubMed: https://pubmed.ncbi.nlm.nih.gov/33206816/
- Wu F, Zhao S, Yu B, Chen YM, Wang W, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020; 579: 265-269. PubMed: https://pubmed.ncbi.nlm.nih.gov/32015508/
- Hashimoto T, Perlot T, Rehman A, Trichereau J, Ishiguro H, et al. ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation. Nature. 2012; 487: 477-481.
- Mao R, Qiu Y, He JS, Tan JY, Li XH, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020; 5: 667-678. PubMed: https://pubmed.ncbi.nlm.nih.gov/32405603/
- Zhang J, Garrett S, Sun J. Gastrointestinal symptoms, pathophysiology, and treatment in COVID-19. Genes Dis. 2021; 8: 385-400.PubMed: https://pubmed.ncbi.nlm.nih.gov/33521210/
- Lin L, Jiang X, Zhang Z, Huang S, Zhang Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 69: 997-1001. PubMed: https://pubmed.ncbi.nlm.nih.gov/32241899/
- Effenberger M, Grabherr F, Mayr L, Schwaerzler J, Nairz M, et al. Faecal calprotectin indicates intestinal inflammation in COVID-19. Gut. 2020; 69: 1543-1544. PubMed: https://pubmed.ncbi.nlm.nih.gov/32312790/
- Burgueño JF, Reich A, Hazime H, Quintero MA, Fernandez I, et al. Expression of SARS-CoV-2 entry molecules ACE2 and TMPRSS2 in the gut of patients with IBD. Inflamm Bowel Dis. 2020; 26: 797-808. PubMed: https://pubmed.ncbi.nlm.nih.gov/32333601/
- Harmer D, Gilbert M, Borman R, Clark KL. Quantitative mRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme. FEBS letters. 2002; 532: 107-110. PubMed: https://pubmed.ncbi.nlm.nih.gov/12459472/
- Xiao F, Tang M, Zheng X, Liu Y, Li X, et al. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020; 158: 1831-1833. PubMed: https://pubmed.ncbi.nlm.nih.gov/32142773/
- Du M, Cai G, Chen F, Christiani DC, Zhang Z, et al. Multiomics evaluation of gastrointestinal and other clinical characteristics of COVID-19. Gastroenterology. 2020; 158: 2298-2301. PubMed: https://pubmed.ncbi.nlm.nih.gov/32234303/
- Luo S, Zhang X, Xu H. Don't overlook digestive symptoms in patients with 2019 novel coronavirus disease (COVID-19). Clin Gastroenterol Hepatol. 2020; 18: 1636-1637. PubMed: https://pubmed.ncbi.nlm.nih.gov/32205220/
- Xu Y, Li X, Zhu B, Liang H, Fang C, et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Medi. 2020; 26: 502-505. PubMed: https://pubmed.ncbi.nlm.nih.gov/32284613/
- Xiong XL, Wong KKY, Chi SQ, Zhou AF, Tang JQ, et al. Comparative study of the clinical characteristics and epidemiological trend of 244 COVID-19 infected children with or without GI symptoms. Gut. 2021; 70: 436-438. PubMed: https://pubmed.ncbi.nlm.nih.gov/32430348/
- Cipriano M, Ruberti E, Giacalone A. Gastrointestinal infection could be new focus for coronavirus diagnosis. Cureus. 2020; 12:PubMed: https://pubmed.ncbi.nlm.nih.gov/32351807/
- Hamming I, Timens W, Bulthuis MLC, Lely AT, Navis GV, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2021; 203: 631-637. PubMed: https://pubmed.ncbi.nlm.nih.gov/15141377/
- Jiao L, Li H, Xu J, Yang M, Ma C, et al. The gastrointestinal tract is an alternative route for SARS-CoV-2 infection in a nonhuman primate model. Gastroenterology. 160: 1647-1661. PubMed: https://pubmed.ncbi.nlm.nih.gov/33307034/
- Singer D, Camargo SM. Collectrin and ACE2 in renal and intestinal amino acid transport. Channels. 2011; 5: 410-423. PubMed: https://pubmed.ncbi.nlm.nih.gov/21814048/
- Zhang H, Wada J, Hida K, Tsuchiyama Y, Hiragushi K, et al. Collectrin, a collecting duct-specific transmembrane glycoprotein, is a novel homolog of ACE2 and is developmentally regulated in embryonic kidneys. J Bio Chem. 276: 17132-17139. PubMed: https://pubmed.ncbi.nlm.nih.gov/11278314/
- Tian Y, Rong L, Nian W, He Y. Gastrointestinal features in COVID‐19 and the possibility of faecal transmission. Aliment Pharmacol Therapeut. 2020; 51: 843-851. PubMed: https://pubmed.ncbi.nlm.nih.gov/32222988/
- Chen Y, Chen L, Deng Q, Zhang G, Wu K, et al. The presence of SARS‐CoV‐2 RNA in the feces of COVID‐19 patients. J Med Virol. 2020; 92: 833-840. PubMed: https://pubmed.ncbi.nlm.nih.gov/32243607/
- Chen L, Li L, Han Y, Lv B, Zou S, et al. Tong-fu-li-fei decoction exerts a protective effect on intestinal barrier of sepsis in rats through upregulating ZO-1/occludin/claudin-1 expression. J Pharma Sci. 2020; 143: 89-96. PubMed: https://pubmed.ncbi.nlm.nih.gov/32173265/
- Fernández-Blanco JA, Estévez J, Shea-Donohue T, Martínez V, Vergara P. Changes in epithelial barrier function in response to parasitic infection: implications for IBD pathogenesis. J Crohn's Colitis. 2015; 9: 463-476. PubMed: https://pubmed.ncbi.nlm.nih.gov/25820018/
- Vandana UK, Barlaskar NH, Gulzar ABM, Laskar IH, Kumar D, et al. Linking gut microbiota with the human diseases. Bioinformation. 2020; 16: 196-208. PubMed: https://pubmed.ncbi.nlm.nih.gov/32405173/
- Duan Y, Prasad R, Feng D, Beli E, Calzi L, et al. Bone marrow-derived cells restore functional integrity of the gut epithelial and vascular barriers in a model of diabetes and ACE2 deficiency. Circulation Res. 2020; 125: 969-988. PubMed: https://pubmed.ncbi.nlm.nih.gov/31610731/
- Pan L, Mu M, Yang P, Sun Y, Wang R, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020; 115: 766-773.PubMed: https://pubmed.ncbi.nlm.nih.gov/32287140/
- Seeliger B, Philouze G, Benotmane I, Mutter D, Pessaux P. Is the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) present intraperitoneally in patients with coronavirus disease 2019 (COVID-19) infection undergoing emergency operations? Surgery. 2020; 168: 220-221. PubMed: https://pubmed.ncbi.nlm.nih.gov/32591139/
- Zhang H, Kang Z, Gong H, Xu D, Wang J, et al. Digestive system is a potential route of COVID-19: an analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut. 2020; 69: 1010-1018. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7211082/
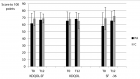
Figures:
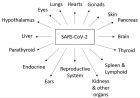
Figure 1
Similar Articles
-
Hypothesis about pathogenic action of Sars-COV-2Del Prete Salvatore*,Marasco Daniela,Sabetta Rosalaura. Hypothesis about pathogenic action of Sars-COV-2. . 2020 doi: 10.29328/journal.ijcv.1001009; 4: 021-022
-
The Psychology of the Common Cold and Influenza: Implications for COVID-19Andrew P Smith*. The Psychology of the Common Cold and Influenza: Implications for COVID-19. . 2020 doi: 10.29328/journal.ijcv.1001011; 4: 027-031
-
Yemen is free of COVID-19Hussein O Kadi*. Yemen is free of COVID-19. . 2020 doi: 10.29328/journal.ijcv.1001012; 4: 032-033
-
Exploring pathophysiology of COVID-19 infection: Faux espoir and dormant therapeutic optionsVinod Nikhra*. Exploring pathophysiology of COVID-19 infection: Faux espoir and dormant therapeutic options. . 2020 doi: 10.29328/journal.ijcv.1001013; 4: 034-040
-
COVID-19: Targeting the cytokine storm via cholinergic anti-inflammatory (Pyridostigmine)Ahmed H Osman*. COVID-19: Targeting the cytokine storm via cholinergic anti-inflammatory (Pyridostigmine). . 2020 doi: 10.29328/journal.ijcv.1001014; 4: 041-046
-
Identifying patterns in COVID-19: Morbidity, recovery and the aftermathVinod Nikhra*. Identifying patterns in COVID-19: Morbidity, recovery and the aftermath. . 2020 doi: 10.29328/journal.ijcv.1001016; 4: 056-064
-
Role of nanotechnology in diagnosing and treating COVID-19 during the PandemicAbdul Baset*,Abdul Waris,Muhammad Ali,Atta Ullah Khan,Asmat Ali. Role of nanotechnology in diagnosing and treating COVID-19 during the Pandemic. . 2020 doi: 10.29328/journal.ijcv.1001017; 4: 065-070
-
COVID-19: The possible medical strategiesMohamed SA Mohamed*. COVID-19: The possible medical strategies. . 2020 doi: 10.29328/journal.ijcv.1001018; 4: 071-075
-
Can house flies mechanically carry and/or transport sars-cov-2?Alfredo Montes*,Wilfrido Coronell,Rosa Baldiris. Can house flies mechanically carry and/or transport sars-cov-2?. . 2020 doi: 10.29328/journal.ijcv.1001019; 4: 076-078
-
Inhaled statins to combat COVID-19 – prophylactic and treatment approachArchana P Iyer*,Maryam A Al-Ghamdi. Inhaled statins to combat COVID-19 – prophylactic and treatment approach. . 2020 doi: 10.29328/journal.ijcv.1001020; 4: 079-080
Recently Viewed
-
Endometriosis as a risk factor for colorectal cancerVíctor Manuel Vargas-Hernández*,José María Tovar- Rodríguez,Víctor Manuel Vargas-Aguilar . Endometriosis as a risk factor for colorectal cancer. Clin J Obstet Gynecol. 2020: doi: 10.29328/journal.cjog.1001057; 3: 093-097
-
Adult Neurogenesis: A Review of Current Perspectives and Implications for Neuroscience ResearchAlex, Gideon S*,Olanrewaju Oluwaseun Oke,Joy Wilberforce Ekokojde,Tolulope Judah Gbayisomore,Martina C. Anene-Ogbe,Farounbi Glory,Joshua Ayodele Yusuf. Adult Neurogenesis: A Review of Current Perspectives and Implications for Neuroscience Research. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001102; 8: 106-114
-
Analysis of Psychological and Physiological Responses to Snoezelen Multisensory StimulationLucia Ludvigh Cintulova,Jerzy Rottermund,Zuzana Budayova. Analysis of Psychological and Physiological Responses to Snoezelen Multisensory Stimulation. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001103; 8: 115-125
-
Sexual Dimorphism in the Length of the Corpus Callosum in CadaverShahnaj Pervin*,Nasaruddin A,Irfan M,Annamalai L. Sexual Dimorphism in the Length of the Corpus Callosum in Cadaver. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001104; 8: 126-129
-
Improvement of the Cognitive Abilities in a Chronic Generalized Anxiety Disorder and Moderate Depression Case using a Novel Integrated Approach: The Cognitome ProgramMohita Shrivastava*. Improvement of the Cognitive Abilities in a Chronic Generalized Anxiety Disorder and Moderate Depression Case using a Novel Integrated Approach: The Cognitome Program. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001100; 8: 069-089
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."