More Information
Submitted: 25 May 2020 | Approved: 11 June 2020 | Published: 12 June 2020
How to cite this article: Iyer AP, Al-Ghamdi MA. Inhaled statins to combat COVID-19 – prophylactic and treatment approach. Int J Clin Virol. 2020; 4: 079-080.
DOI: 10.29328/journal.ijcv.1001020
Copyright License: © 2020 Iyer AP, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Inhaled statins to combat COVID-19 – prophylactic and treatment approach
Archana P Iyer* and Maryam A Al-Ghamdi
Department of Biochemistry, Science College, King Abdul Aziz University, Jeddah, Saudi Arabia
*Address for Correspondence: Archana P Iyer, Department of Biochemistry, Science College, King Abdul Aziz University, Jeddah, Saudi Arabia, Email: [email protected]
The coronavirus disease 19 (COVID-19) is a highly transmittable and pathogenic viral infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which emerged in Wuhan, China and spread around the world (WHO, 2020). The genome of the SARS-CoV-2 has been reported over 80% identical to the previous human coronavirus (SARS-like bat CoV) [1]. As of May 2020, more than 5 million people have been affected worldwide with deaths amounting to 333000, the numbers increasing at an alarming rate day by day.
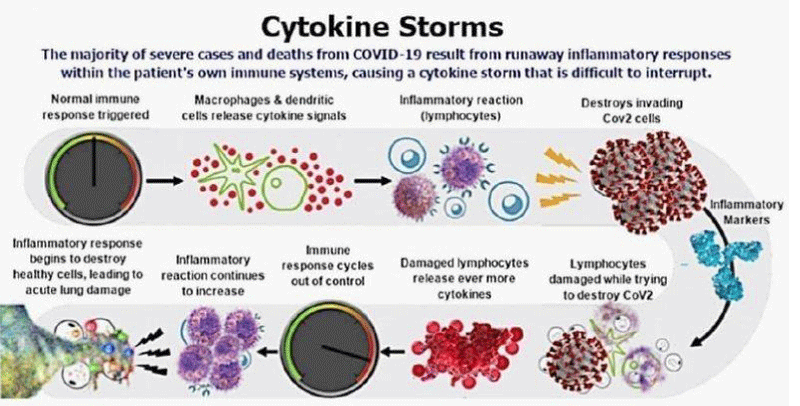
COVID-19 complications–the cytokine storm (Figure 1)
Current management of COVID-19 is supportive, and respiratory failure from acute respiratory distress syndrome (ARDS) is the leading cause of mortality. With multiorgan failure. In adults, sHLH is most commonly triggered by viral infections and occurs in 3·7% – 4·3% of sepsis cases [2]. Secondary haemophagocytic lymphohistiocytosis (sHLH) is an under-recognised, hyperinflammatory syndrome characterised by a fulminant and fatal hypercytokinaemia.
Cardinal features of sHLH include unremitting fever, cytopenias, and hyperferritinaemia; pulmonary involvement (including ARDS) occurs in approximately 50% of patients. A cytokine profile resembling sHLH is associated with COVID-19 disease severity, characterised by increased interleukin (IL)-2, IL-7, granulocyte-colony stimulating factor, interferon-γ inducible protein 10, monocyte chemoattractant protein 1, macrophage inflammatory protein 1-α, and tumour necrosis factor-α [3].
Figure 1: Cytokine Storm.
Current therapeutic strategies against COVID-19
Initially, interferons-α nebulization, broad-spectrum antibiotics, and anti-viral drugs were used to reduce the viral load, however, only remdesivir has shown promising impact against the virus. Remdesivir only and in combination with chloroquine or interferon beta significantly blocked the SARS-CoV-2 replication and patients were declared as clinically recovered [4]. Various other anti-virals are currently being evaluated against infection. Nafamostat, Nitazoxanide, Ribavirin, Penciclovir, Favipiravir, Ritonavir, AAK1, Baricitinib, and Arbidol exhibited moderate results when tested against infection in patients and in vitro clinical isolates (Sheahan, et al. 2020). Recently in Shanghai, doctors isolated the blood plasma from clinically recovered patients of COVID-19 and injected it in the infected patients who showed positive results with rapid recovery [5].
Current hypothesis: Statins as aerosols to combat COVID-19
Statins are inhibitors of the rate‐limiting enzyme, 3‐hydroxy‐3‐methylglutaryl coenzyme A (HMG‐CoA) reductase in cholesterol biosynthesis (fat synthesis within human body tissues and blood). Statins act primarily via effects on lipids, by inhibiting the intracellular synthesis (synthesis inside the body cells) of L‐mevalonic acid and its metabolites. The overall cascade of mechanisms in the mevalonate pathway contributes to a reduction in serum cholesterol levels. Statins are proven to have highly significant anti inflammatory properties.
1. Some of the mechanisms responsible for the anti‐inflammatory effects include: reduction of pro‐inflammatory cytokines by inhibiting mRNA signalling pathways
2. inhibition of lymphocyte proliferation by reduction of cytokine levels
3. production of anti‐oxidant effects through inactivation of reactive oxygen species (ROS)
4. up‐regulation of endothelial nitric oxide synthase expression
5. reduction of bronchial smooth muscle proliferation in response to mitogens
Statins “pleiotropic” anti-inflammatory property has often propelled the research into utility against asthma.
The current hypothesis is to use statins to control the cytokine storm induced by the viral load in the lungs. Statins have already been successfully tested in animal models against other influenza viruses. Furthermore there are studies that have shown that patients who had been regularly taking statins had a faster recovery rate from flu and also exhibited lower mortality rates. In essence the statins facilitate faster recovery from the viral pneumonia by significant anti inflammatory effect, slowing down the damage to the lungs and facilitating recovery without reaching the stage of being put on ventilators.
The hypothesis is built on two modalities
Prophylactic treatment for healthcare workers that would prevent them from getting infected as well as transmitting the infection
Adjunct therapy for patients along with antiviral drugs already in use for treatment.
The Premise
The premise for using statins against COVID is based on how soap kills the virus. The virus contains an outer lipid membrane that holds the cell contents intact. Soap interacts with the lipid membrane and destroys it, thereby disintegrating the protective lipid layer, leading to fall out of the cell contents. This is the reason frequent hand washing with soap is recommended to kill the virus. This is the premise for the hypothesis of directly delivering statins to the site of viral infection, so that the fat solubilising statins literally mimic the effect of soap in the lungs. Once in the blood stream, statins can have biochemical effects that vary from person to person based on their HDL and LDL levels. Whereas, delivering the virus directly to the lungs which is the site of major damage caused by the virus, would help in localized killing of the pathogen, having no bearing on the patient’s lipid profile.
The main focus would be to deliver the statins in two forms: as a nasal spray and as an inhaler.
Since the virus attacks and lodges on to the mucus membrane lining of the nasal passage as well as the throat, administering the statins as a nasal spray as well as inhaler to patients showing initial symptoms would directly reach the viruses at the site of infection and destroy them. The mode of action of statins as lipid degraders would facilitate direct destruction of the lipid membrane of the virus thereby causing death of the virus leading to reduced viral load. This in turn would not elicit a rapid immune response that usually leads to the cascading cytokine storm effect.
Of the various statins available, rosuvastatin and simvastatin have been found to be highly effective anti-inflammatory compounds against viral influenza.
This being the hypothesis, the target is to formulate the right dosage of the ideal statin and deliver it as a spray and inhaler. Statins have been earlier formulated in the form of aerosols and tested on animal models against flu viruses. The challenge is to arrive at the right dosage and the most effective deliverable form.
Envisaged beneficial effects
Aerosolized statins would directly reach the virus in the nasal cavity as well as the lungs, kill them at the site of infection. It is well established that the devastation caused by COVID is mainly attributed to the extreme immune and inflammatory response elicited by the virus, thereby creating a cytokine storm that causes extensive damage to the lung cells, forcing the patient to be put on ventilators. The above formulated aerosolized statins would kill the virus at the site of infection, reduce the viral load, thereby slowing down the drastic release of immune modulators. The already established anti inflammatory and cardio protective effects of statins would be an added advantage in this therapy.
- Mousavizadeh L, Ghasemi S. Genotype and phenotype of COVID-19: Their roles in pathogenesis [published online ahead of print, 2020 Mar 31]. J Microbiol Immunol Infect. 2020; S1684-1182 (20) 30082-7. PubMed: https://pubmed.ncbi.nlm.nih.gov/32265180/
- Hutchinson M, Tattersall RS, Manson JJ, Haemophagocytic lymphohisticytosis—an under recognized hyper inflammatory syndrome. Rheumatology. 2019; 58: vi23–vi30
- Huang C, Wang Y, Li X, Ren L, Zhao J, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395: 497-506. PubMed: https://pubmed.ncbi.nlm.nih.gov/31986264/
- Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. The Lancet. 2020.
- Derebail VK, Falk RJ. ANCA-associated vasculitis—refining therapy with plasma exchange and glucocorticoids. N Engl J Med. 2020; 382: 671-673. PubMed: https://pubmed.ncbi.nlm.nih.gov/32053306/